
Dental Implant Coding Guidelines: Get Procedure Codes for Providers
Implants and the procedures associated with them are not covered benefits under most Delta Dental plans. But when implant services are covered, most denials are because of coding errors rather than a lack of coverage.
Let’s take a look at some common reasons for denials for implants and the procedures and prostheses associated with them.
Prefabricated abutment vs. custom fabricated abutment
Prefabricated abutments and custom fabricated abutments use separate codes:
- D6056: Prefabricated abutment — includes modification and placement
- D6057: Custom fabricated abutment — includes placement
Prefabricated abutments are machine made and may require modification, while custom fabricated abutments are created by a laboratory process and are specific for an individual application.
Abutment-supported vs. implant-supported crowns
Abutment-supported crowns use a prefabricated abutment (D6056) or a custom fabricated abutment (D6057) to attach a prosthetic crown to the implant body. Abutment-supported single and fixed partial denture crowns require the submission of accompanying abutment codes.
Implant-supported crowns attach directly to the implant body without an abutment. Implant-supported single and fixed partial denture crowns do not require the submission of accompany abutment codes.
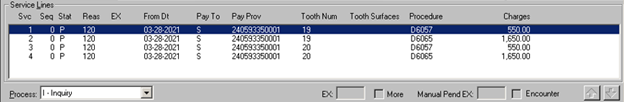
The following image contains an example of incorrect coding. In it, the dental office submitted custom fabricated abutments (which are coded D6057) with implant-supported crowns (coded D6065) for teeth #19 and 20. But implant-supported crowns are not attached to the implant with an abutment, so the procedures should have been coded as abutment-supported crowns.
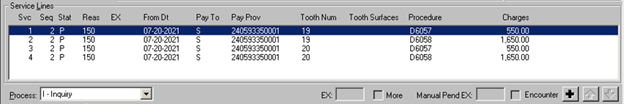
In the following correctly coded image, the dental office submitted custom fabricated abutments (D6057) with abutment-supported crowns (D6058) for teeth #19 and 20 implant supported crowns, which are attached to the implant using an abutment.
If you receive a denial for abutment-supported or implant-supported crowns, it may be one of the following:
- 161. Benefits could not be determined because of missing/conflicting information
- 7C2. The submitted procedure is not payable due to the absence or conflict of a related service.
- 9WA. The fee for this procedure is considered to be part of, and included in the fee for, a completed service.
Single implant crowns vs. fixed partial denture implant crowns
A prosthetic crown that is used to restore one implant is known as a single implant crown. A prosthetic crown that is attached to an implant and is used as a bridge anchor to replace missing teeth is known as a fixed partial denture implant crown.
Here is an example of incorrect coding for these crowns.
| Tooth | Code |
| #29 | D6065 (incorrect) |
| #30 | D6245 |
| #31 | D6065 (incorrect) |
In this example, the coding is incorrect because the abutments on teeth #29 and 31 are coded as single crowns. For this restoration, the following coding is correct:
| Tooth | Code |
| #29 | D6075 (correct) |
| #30 | D6245 |
| #31 | D6075 (correct) |
Here, the abutments on teeth #29 and 31 are correctly coded as fixed partial denture crowns.
Natural tooth single crown and fixed partial denture retainer crown codes are often used in error to code implant-supported prosthetics. Instead, they should be coded as fixed partial denture implant crowns.
| Incorrect, coded as natural teeth | Correct, coded as implants |
| D6740, #29 (incorrect) D6056, #29 D6245, #30 D6740, #31 (incorrect) D6056, #31 |
D6068, #29 (correct) D6056, #29 D6245, #30 D6068, #31 (correct) D6056, #31 |
If you receive a denial for single implant or fixed partial denture implant crowns, it may be one of the following:
- 161. Benefits could not be determined because of missing/conflicting information
- 7C2. The submitted procedure is not payable due to the absence or conflict of a related service.
- 9WA. The fee for this procedure is considered to be part of, and included in the fee for, a completed service.
Alternate benefits when there is no implant coverage
Delta Dental’s standard plans pay an allowance or alternate benefit towards the cost of implant-supported prosthodontic appliances, subject to the same limitations as standard prosthodontic services. The allowance is based on the fee for a standard pontic procedure. The patient is responsible for any difference in the cost of the implant-supported procedure.
Denial codes for alternate benefits when there’s no implant coverage may be one of the following:
- FLM. An alternate procedure/benefit has been applied.
- 503. This service isn’t a covered benefit of the enrollee’s program. An alternate procedure/benefit has been applied.
Congenitally missing teeth
Implant placement will not be considered for the replacement of congenitally missing permanent teeth or for the correction of other developmental or congenital defects resulting in spacing due to migration or drifting of teeth.
Denial codes for congenitally missing teeth implant placement may include the following:
- 511. Procedures to correct congenital or developmental malformations are not covered.
Associated denials related to implant procedures
X-rays
Pre-operative x-rays depicting each implant site are required to determine the payment of benefits on pre-authorizations. Post-operative x-rays of implant placement are required to determine payment of benefits on paid claims and must depict the entire implant. Implant length, width and location must be appropriate for the clinical condition and allow for adequate function of the implant-supported restoration/prosthesis.
Denial codes for x-rays may include the following:
- 570. Benefits could not be determined because of missing pre-operative radiographic images.
- 586. Benefits could not be determined because of missing post-operative radiographic images.
- 5RX. Benefits could not be determined because the submitted radiograph does not depict the entire tooth.
- 569. Benefits could not be determined because of the non-diagnostic nature of the radiographic images submitted.
Re-cementation of implant prosthetics
The code D2920 (re-cement or re-bond natural tooth crown) is often used in error to code re-cementation of implant prosthetics. The appropriate implant crown recement codes are as follows:
- D6092 – Re-cement or re-bond implant/abutment supported crown
- D6093 – Re-cement or re-bond implant/abutment supported fixed partial denture
Denial codes for re-cementation may include the following:
- 788. A benefit allowance cannot be made for the requested procedure as our records show that this tooth was previously extracted.
- 161. Benefits could not be determined because of missing/conflicting information.
Edentulous arches
For a completely edentulous arch, replacement of teeth and restoration of the occlusion can be adequately restored with four to six dental implants.
D6190 – Radiographic/surgical implant index, by report
When your patients’ plans include implant benefits, Delta Dental considers the fee for procedure D6190 to be included in the fee for the definitive treatment for one implant. A separate fee may not be charged to the patient or Delta Dental. Under contracts with implant coverage, procedure D6190 may be covered at the prosthetic benefit level when two or more implants are placed during the same treatment episode. If implants are not covered by the patient’s plan, this procedure is not a benefit, and the patient is responsible for the fee.
Denial codes related to D6190 may include the following:
- 9WA. The fee for this procedure is considered to be part of, and included in the fee for, a completed service.
- 7BB. This service is not a covered benefit of the enrollee’s plan.
D6011 – Second stage implant surgery
When implant services are covered by the patient’s contract, Delta Dental considers the fee for this procedure to be included in the fee for procedure D6010, surgical placement of implant body. A separate fee may not be charged to the patient or Delta Dental.
Denial codes related to D6011 may include the following:
- 9WA. The fee for this procedure is considered to be part of, and included in the fee for, a completed service.
- 718. This fee for this procedure is considered to be part of, and included in the fee for, a completed service.
D6199 – Unspecified implant procedure, by report
Please provide a narrative report with a complete description of the procedure and its rationale. Tools used, parts, healing caps, etc. will be considered inclusive in the implant procedure and not a separate benefit.
Denial codes related to D6199 may include the following:
- 564. Submit clinical treatment narrative.
- 9WA. The fee for this procedure is considered to be part of, and included in the fee for, a completed service.
Delta Dental’s processing policies for implants and the procedures and prostheses associated with them should be considered guidelines. Whenever an exceptional case is involved, please provide a full narrative description and any available supporting documentation to help our staff determine benefits. To ensure timely benefit determination, always submit the appropriate supporting documentation on your initial submission.
Recent posts
- Oral health care for seniors: Improving access, improving outcomes
- Simplify your credentialing with CAQH: Check out our webinar recordings
- Updated 2026 CDT codes are here
- View our CDT 2026 Updates webinar and stay on top of code changes
- EFT will become our standard payment method starting 1/1/27
- Start the year strong: Key reminders to support your practice in 2026
- Discover 3 tips to power up your practice with new workflows
- Updated 2026 CDT codes are here
- Partner with us to improve the health outcomes of our shared members
- Say hello to our 2026 Medicare Advantage DHMO partners
