Orthodontic Codes & Billing Guidelines for Providers

Wondering what you need to submit with your claim? Straighten out your claims with this list of frequently asked questions about orthodontic claims! No need to brace yourself for claim rejections, though! Use this handy guide to submitting orthodontic claims and you’ll be an ortho pro in no time.
How do I submit an orthodontic claim online?
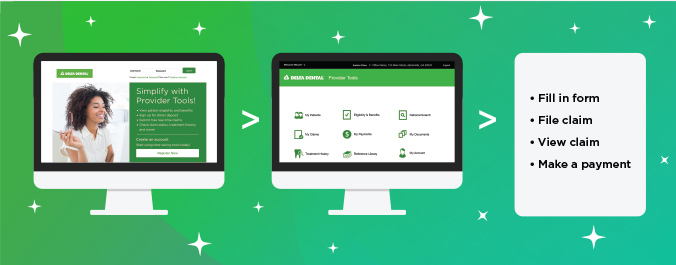
You can submit claims online through Provider Tools. Register for an account, log in to your dashboard and select Submit claim. You only need to submit one claim at the time of the initial banding.
There’s no need to submit additional claims for monthly adjustments. Delta Dental calculates payment based on that first claim with complete treatment and fee information.
You can keep track of your claims by selecting My claims in the Provider Tools dashboard.
What information do I need to include on an orthodontic claim?
You can refer to pages 5–4 and 5–5 in our dentist handbook for general Delta Dental policy around orthodontic claims. Each plan may require different information, so make sure to look at your patient’s coverage in Provider Tools for specific requirements. While you’re there, you can also submit and track claims using the Submit claims and My claims tools!
For orthodontic claims, submit a single claim at the time of the initial banding with the following information:
- a description of the dentition
- the procedure code with a description of appliance and treatment
- the banding date and estimated number of active treatment months
- the total fee you intend to collect for services (including the initial down payment and monthly fee)
If applicable, you should also include the amount paid by a previous dental carrier, the name and procedure code of appliances used to control a harmful habit and any dual coverage information. You don’t need to submit x-rays or radiographs for claims unless specifically asked to do so by Delta Dental.
How are orthodontic claims paid?
Our allowances for orthodontic procedures include all appliances, adjustments, insertion, removal and post-treatment stabilization (retention). Calculations are based on the all-inclusive total treatment plan amount, subject to any deductible, the appropriate payment percentage and maximum amount.
Our first payment is 50% of the total amount payable. The remaining 50% is paid 12 months later.
For most plans, the orthodontic maximum is a lifetime maximum. Also, if the total amount payable is $500 or less, we pay the full amount in one payment when the claim is processed
Are there exceptions to the two-payment schedule?
Yes. If the patient’s plan has specific provisions for a different payment method, we will pay accordingly. Also, if treatment ends before our second payment is due, advise us that the bands were removed and the treatment has been completed. You may call Customer Service or submit a claim that includes this information.
How should fees for x-rays and study models be submitted?
Submit fees for these records along with the banding information or on a separate claim. If submitted separately, indicate on the claim that these records are in conjunction with orthodontic treatment. You don’t need to x-rays or study models to Delta Dental unless specifically requested.
Are retainers and harmful habit appliances covered?
Yes. Allowances include all appliances, adjustments, insertion, removal and post-removal stabilization (retainers).
Harmful habit appliances are covered if a patient’s plan includes a specific provision for minor treatment to control harmful habits. The provision must be in conjunction with orthodontic treatment (procedure code D8210) and/or separately (procedure code D8220).
Retainer repairs and replacements are not covered.
How do I submit claims for Invisalign, lingual braces or SureSmile?
Some plans cover alternative appliances like Invisalign, lingual braces or SureSmile. You can check if your patient’s plan covers clear aligners by visiting Provider Tools, clicking on My patients and selecting Check eligibility and benefits next to the name of the patient. Click Orthodontics under Benefit details to view limitations, age limits and coverage levels. There is no unique procedure code for clear aligners, so reference the CDT codes used for conventional treatments, D8010 through D8090.
Submit claims for clear aligners as a separate line item from the orthodontic treatment code and fee. Make sure to enter a complete description of the service, including reference to Invisalign, lingual braces or SureSmile.
How is payment determined when a patient switches to a new orthodontist?
We calculate remaining benefits based on the date of the first adjustment with the new orthodontist. The new orthodontist should submit a claim using the first adjustment date as the starting date of treatment, along with a notation that the patient has transferred from another office.
Are orthodontic benefits ever prorated? How?
Yes. Prorating occurs when an event affects the patient’s orthodontic coverage. New Delta Dental coverage after treatment has begun, an increase in existing coverage, a change in eligibility or a change of orthodontists might spur proration.
When Delta Dental prorates payments, we subtract the total fees for any treatment months that occurred before the patient’s effective date with Delta Dental from the total orthodontic treatment fee. Our amount payable is then based on the remaining treatment fee, the remaining number of treatment months and applicable payment percentage and maximums.
Why was my claim rejected?
Claims can be rejected for a variety of reasons. The most common rejections are for incorrectly entered patient information, like enrollee IDs or patients submitted as dependents. Make sure to include all relevant information on your claims, like multiple banding dates, multiple case fees and the correct length of treatments. Excluding this information may lead to a rejected claim We also see rejections for claims using CDT codes that have been deleted or revised, so stay on top of the latest CDT updates!
Recent posts
- Dr. Carlos Cruz — serving a community in need with cleft and craniofacial expertise
- Parent-approved ways to help calm anxious pediatric patients
- Oral health care for seniors: Improving access, improving outcomes
- Simplify your credentialing with CAQH: Check out our webinar recordings
- Updated 2026 CDT codes are here
- View our CDT 2026 Updates webinar and stay on top of code changes
- EFT will become our standard payment method starting 1/1/27
- Start the year strong: Key reminders to support your practice in 2026
- Discover 3 tips to power up your practice with new workflows
- Updated 2026 CDT codes are here
